- Monday, 16 February 2026
Scaling Up TB Free Initiative
Globally, TB is a major public health challenge. However, TB is preventable and usually curable disease. Caused by the bacillus Mycobacterium tuberculosis, it is spread when people who are sick with TB expel bacteria into the air. About a quarter of the global population is estimated to have been infected with TB. Drug-resistant TB continues to be a serious public health threat. More importantly, TB is a social disease and its understanding demands profound impacts of historical, social, cultural, and economic on individuals and communities. Needless to say, TB is a disease of poverty with prolonged socio-economic distress, vulnerability, marginalisation, stigma and discrimination. Therefore, it is necessary to consider differential effects of TB in terms of socio-economic status, gender, migration, and other socio-demographic variables.
Considering the urgency of effective and sustained TB response, National TB Control Centre (NTCC) has been consistently implementing National TB Programme (NTP) with the additional technical support from WHO, Global Fund, and other implementing partners at all levels. Over the years, the NTCC has been proactively engaged in formulating policies, strategies, and relevant technical guidelines to ensure quality assurance as well as scaling up research and innovations for sustained national TB response.
Development challenge
Ending TB is not just a public health problem, but a development challenge. Therefore, national strategic plan to end TB (2021/22-205/26) has largely focused on integrated patient-centred care and prevention which aims to ensure early detection, treatment and prevention for all TB patients including children. Moreover, it is necessary to ensure all people have equal and unhindered access to affordable services, and they engage in their care.
Likewise, there are significant efforts to strengthen health and social sector policies and supportive systems by accelerating the progress on Universal Health Coverage (UHC), social protection and regulatory frameworks for case notification, vital registration, quality and rational use of medicines, and infection control. In addition, the strategic priorities also focus on operational research for the design, implementation, and scaling-up of innovations. In this context, TB free initiative is one of the strategic priorities to make the local governments more accountable towards the ambitious target of ending TB. The NTCC has developed a comprehensive guideline for TB free initiative to effectively plan and implement activities related to active TB case finding, diagnosis, prevention, treatment, care and support in the federal context.
This clear shows Nepal’s strong political commitment for implementation of the TB free initiative to ensure all people with TB have access to quality care through the UHC. The initiative also aims to strengthen community engagement for the meaningful participation of TB patients, promotion of human rights and patient support in national response. While there are significant efforts to include TB patients and their families in health insurance package and social protection services, it is important to address the social determinants of TB and focus interventions for vulnerable groups such as very poor, people living with HIV, diabetes, disability and migrants.
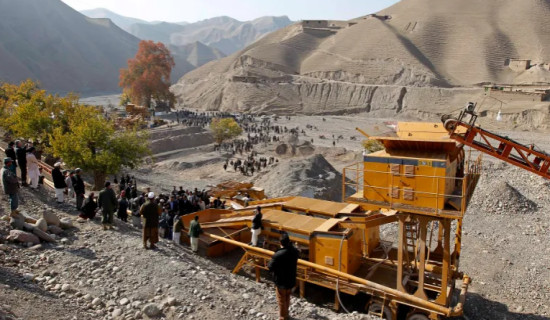
Therefore, one of the important features of TB free initiative is to enhance political leadership, commitment, ownership, multi-sector engagement and partnership for a coordinated response to end TB. While there is still a funding gap for the NTP, local governments can prioritise their resources for continuity and sustainability of TB services. As of now, the TB free initiative is implemented in 25 municipalities and it will be scaled up in additional 100 municipalities soon.
In order to ensure participatory and inclusive planning and implementation of TB free initiative, there are specific committees responsible for providing technical support in micro-planning for multi-sector actions at all levels. However, there is critical need to strengthen the capacity of local governments and the committees in developing a profile of TB patients, micro-planning, resource mobilisation, monitoring and evaluation of TB diagnosis, prevention, treatment, care and support. Undoubtedly, TB free initiative demands sustained political commitment, meaningful community engagement, respect for human rights, gender inclusion and equity considerations. Within local health systems, it is important to ensure provision of high quality integrated care to all patients with TB, including diagnostics and treatment services across public and private sectors. Integrating TB services help gain efficiency and access to treatment and care.
Multi-sectoral action
As TB is driven by social, cultural and economic determinants, multi-sectoral action is necessary to address them through community-led interventions. This also generates local evidence to strengthen TB response in the communities. Beyond health sector, it is necessary to establish a multi-sector accountability framework for coordinated actions with all sectors. Working with civil society is instrumental in strengthening community engagement and leveraging their capacities to end TB. Furthermore, people affected by TB can play key role in implementation of TB free initiative at community level.
During COVID-19 pandemic and other disasters, the civil society and their networks in the communities have played critical role in maintaining access to essential health care. Recovery from the pandemic and other health emergencies during disasters demands resilient communities to realistically face complex livelihood challenges and rebound from the huge number of missing people with TB due to the disruptions. Additionally, the use of digital technologies can be helpful to support psychosocial well-being, patient rights, and adherence to TB treatment and improve better health outcomes. Reaching out to key and vulnerable populations should be one of the key strategies of the TB free initiative to effectively address the structural inequalities and barriers they face in accessing TB services for years.
(Bhandari is a health policy analyst)