- Saturday, 2 August 2025
Fungal Infection Of Nails
Fungal infection of the nails also known as onychomycosis is one of the most common disorders of the nails. It usually affects the elderly with around 40% of elderly individuals suffering from the disease. Males are more commonly affected than females. The predisposing factors include diabetes mellitus, immunosuppression due to HIV or drugs and peripheral arterial disease. Toenails are involved more commonly than fingernails.
Clinical features:
There are many types of onychomycosis, the most common of which is distal and lateral subungual onychomycosis (DLSO) (figure 1).
One or both the big toe nails are the first to be affected. It usually occurs in association with interdigital tinea pedis, which is commonly called in Nepali (figure 2). The main features of DLSO are nail plate that is detached from the underlying nail bed, yellowish white discolouration of the nail plate and presence of debris underneath the nail plate.
The second type of fungal infection of the nail called white superficial onychomycosis (WSO) presents with white opaque formations on the nail plate that can be scraped away. Proximal subungual onychomycosis (PSO) is a rare type of fungal infection of the nail that usually occurs in individuals with HIV infection. It involves the area of the nails near its attachment to fingers and presents as white area under the proximal nail plate. When DLSO or PSO are ignored, it may result in total dystrophic onychomycosis (TDO) where almost all the nails are thickened and yellowish to whitish in colour (figure 3).
Diagnosis:
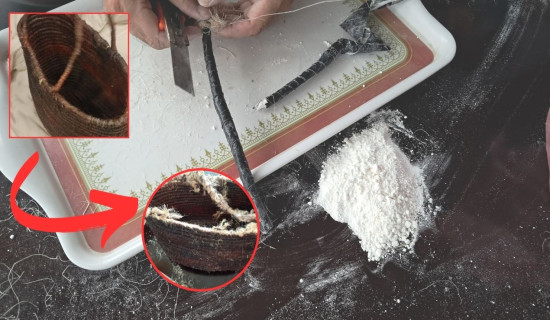
Although many new technologies have emerged in the last few years for diagnosing this condition, the two most commonly used techniques are potassium hydroxide (KOH) mount and nail culture. For the first technique, nail material is immersed in a solution of 40% KOH. This strong alkali will dissolve the nail plate but the fungus remains intact. The material is then transferred to a slide and observed under the microscope to look for fungal elements. Although this method allows clinicians to detect fungal elements, it does not allow us to recognize the type of fungus causing the onychomycosis.
To identify the type of fungus, a culture is needed. This technique involves transferring the infected nail material to an appropriate culture medium for development and observation of characteristic fungal colonies. Histopathology of nail clippings also allows visualization of fungal elements using a special stain called periodic acid-Schiff (PAS) stain.
Treatment:
Proper treatment of fungal nail infections requires both systemic and topical therapy. Systemic therapies are more effective but can be limited by drug interactions and possibility of liver toxicity. Topical therapies should not be advocated as solo therapy as they have limited efficacy without nail plate debridement.
The only topical therapy currently available in Nepal is amorolfine 5% nail lacquer, which can be applied once weekly. Topical agents available in other countries include ciclopirox nail lacquer, efinaconazole 10% solution, tavaborole 5% solution and luliconazole 10% solution. For topical therapy to be effective, the nail bed should initially be debrided. Debridement can be carried out by spatula provided with the topical medication. Even after successful therapy with topical agents, re-infections and recurrences can be observed in up to 25% of patients. Treatment duration is for 6-12 months.
The systemic agents for the treatment of fungal nail infections include oral itraconazole capsule and terbinafine tablet. The reasons for systemic therapy include total dystrophic
onychomycosis, very thick nail plates with subungual debris, infection with rarer varieties of fungi, treatment failure with topical agents and patients with co-morbidities such as diabetes mellitus, peripheral arterial disease and immunosuppression.
Itraconazole capsules are preferred over terbinafine tablets when the fungi causing the infection belong to species other than the common ones. Their proper use can lead to complete cure in 90% of fingernail and 80% of toenail fungal infections.
The treatment duration is 2 months for fingernails and 3 months for toenails.
However, complete recovery can take up to 9 months for fingernail and 18 months for toenail infections. Periodic removal of affected nail plate can accelerate improvement. As with topical therapy, re-infections and recurrences may be seen in up to 20% of patients.
Important Tips
Nowadays, a lot of advertisements are put on social media including Facebook advocating the use of special solutions for instant treatment of fungal infection of nails with money back guarantees. These solutions are said to contain argan oil, tea tree oil, cloves and rosemary oil. Argan oil, while effective as a nail moisturizer has been reported to cause allergic reactions in the nails. Tea tree oil and cloves oil are mentioned as home therapies for treatment of onychomycosis but the concentration and duration of treatment have not been standardized. Scientific studies have not advocated the use of rosemary oil as a therapy for onychomycosis. We would advise patients to refrain from choosing these therapies as they are neither evidence based nor time tested.
Home remedies for preventing and treating onychomycosis include regular washing of feet followed by thorough drying. Antifungal powders can be applied after drying. Nails should be trimmed regularly and nail clippers should be disinfected after use. Open shoes should be preferred over closed tight ones whenever possible. Socks should be changed once daily and sweat absorbing cotton or other natural fibre made socks should be preferred over synthetic ones. A balanced diet rich in protein, iron, biotin and other micro minerals are should be taken to support nail regrowth and prevent the formation of brittle nails.
Fungal infections of the nails should be taken seriously as ignoring them may lead to severe involvement of all twenty nails resulting in unsightly appearance. We recommend patients to visit their dermatologists for the treatment of their condition.
(The writier is a dermatologist, venereologist and leprologist. bibush.amatya@gmail.com)